Sinus tachycardia
Sinus tachycardia – increase in heart rate from 95 to 125 per minute while maintaining the correct sinus rhythm. It is based on an increase in automaticity in primary pacemaker the sinoatrial node.
Table of Contents
ToggleCauses: various endogenous and exogenous influences: physical activity and mental stress, emotion, infection and fever, anemia, hypovolemia and hypotension, respiratory hypoxemia, acidosis and hypoglycemia, myocardial ischemia, hormonal disorders (thyrotoxicosis), drug effects, heart failure.
RHYTHM DISTURBANCES OF THE HEART
Arrhythmias in the broadest sense of the word according Kushakovskij M.S. are the blockades, and ectopic beats and tachycardias. Modern
electrophysiology, considering arrhythmias as an independent science, includes in this concept only true arrhythmias, i.e. violations of excitability, but not conductivity violations.
The exact causes of arrhythmias are still unknown. There are only experimental electrophysiological models. The arrhythmia may be primary disease of the heart and can be a complication of other heart diseases (heart attacks, cardiomyopathy, myocarditis, valvular, electrolyte changes). Rarely arrhythmias may occur with the neuro-endocrine and gastrointestinal diseases.
Classification of arrhythmias
01.Nomotopic arrhythmias -(associated with changes of sinus node automaticity):
1) Sinus tachycardia;
2) Sinus bradycardia;
3) Sinus arrhythmia;
4) Rigid sinus rhythm
02.Heterotopic or ectopic arrhythmias.
A – Passive heterotopic
1) Atrial rhythms
2) Nodal rhythms
3) Ventricular (idioventricular) rhythms;
4) Migration pacemaker on the Atria.
B – Active heterotopic:
1) Extrasystole
2) Paroxysmal tachycardia
3) Atrial and ventricular fibrillation and flutter.
03.Combined rhythm disturbances:
1) Parasystole;
2) AV dissociation.
01.SINUS TACHYCARDIA
Sinus tachycardia – increase in heart rate from 95 to 125 per minute while maintaining the correct sinus rhythm. It is based on an increase in automaticity in primary pacemaker the sinoatrial node.
Causes: various endogenous and exogenous influences: physical activity and mental stress, emotion, infection and fever, anemia, hypovolemia and hypotension, respiratory hypoxemia, acidosis and hypoglycemia, myocardial ischemia, hormonal disorders (thyrotoxicosis), drug effects, heart failure.
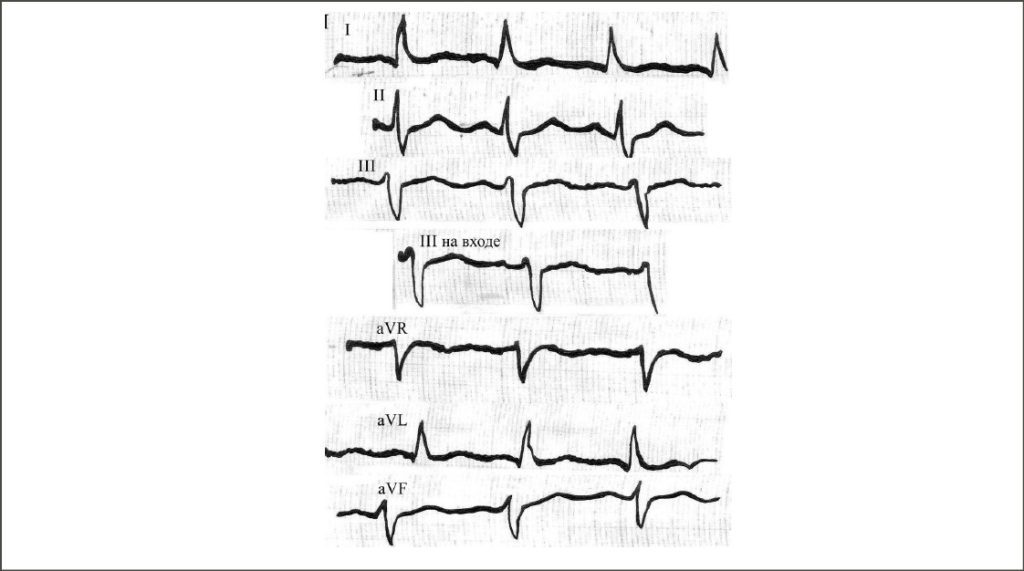
ECG signs:
the P wave of sinus origin (positive in I, II, aVF, V4-6; negative in aVR);
shortening of all intervals (PQ, RR, etc.) compared to the norm;
the difference between intervals R-R does not exceed 0.15, but most of 0,05;
QRS; – the presence of unchanged QRS complex;
possible shift of ST segment below the isoline of “anchor type”;
change the morphology of the P wave the type of “pulmonale”.
0.2 SINUS BRADYCARDIA
Sinus bradycardia – a decrease in heart rate less than 50 per minute while maintaining the correct sinus rhythm. Sinus bradycardia is due to decreased automaticity sinoatrial node.
Reasons- The main cause of sinus bradycardia is the increase of vagal tone. Normal often occurs in athletes, however, can occur in various diseases (myxedema, coronary heart disease, peptic ulcer disease, typhoid, intracranial hypertension, etc.).
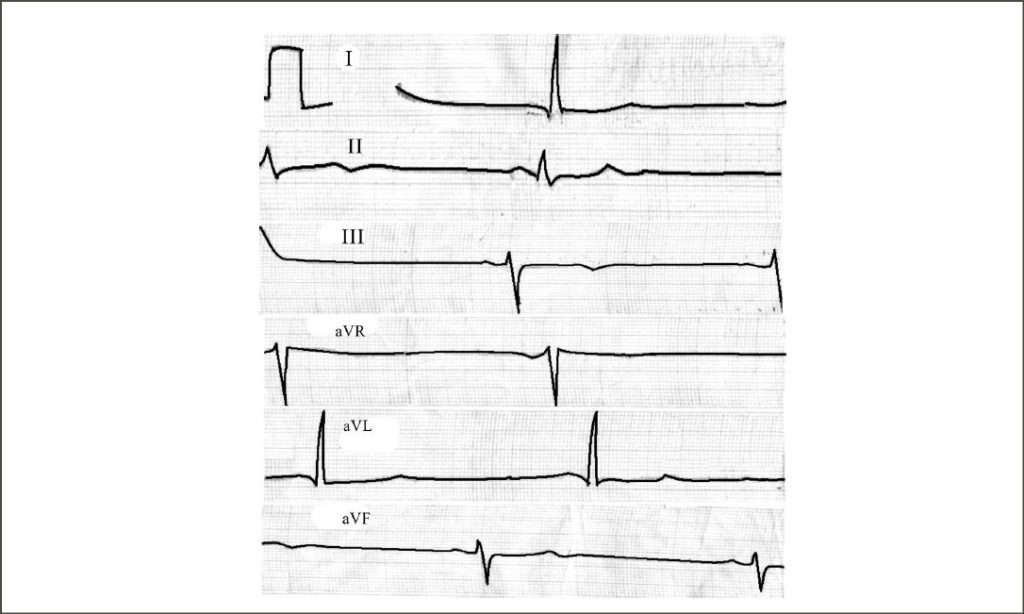
SINUS BRADYCARDIA ECG signs:
1) the P wave of sinus origin (positive in l, II, aVF, V4-6; negative in aVR);
2) the elongation of all intervals in comparison with the norm;
3) the difference between the intervals R-R does not exceed 0.15;
4) the presence of unchanged QRS complex;
5) possible lifting ST up to 1 mm. Above the contours;
6) change the morphology of the P wave according to the “mitrale”.
Also Read this Article
Doctor कैसे बने जाने सब कुछ हिंदी में
03.Sinus arrhythmia
Sinus arrhythmia – irregular sinus rhythm, characterized by periods of gradual increase and shortening of the rhythm.
Reasons– Sinus arrhythmia is due to irregular impulses in the sinoatrial node, caused by an imbalance of the autonomic nervous system
with a distinct predominance of its parasympathetic division.
Most common respiratory sinus arrhythmia, in which heart rate increases on inspiration and decreases on exhalation. Respiratory sinus arrhythmia is a manifestation of the norms in children and adolescents up to 15 years, pregnant women and in individuals of the asthenic Constitution. Specific treatment is not required.
There is an acyclic (not respiratory) sinus arrhythmia, which does not disappear on the breath. It occurs mainly in older patients (over 60 years of age) with severe atherosclerosis of the coronary and cerebral arteries.
ECG signs (common to all types):
-the P wave of sinus origin (positive in I, II, aVF, V4-6; negative in aVR);
-the difference between the intervals of R-R exceeds 0.15, but not more than 0.20;
-the presence of unchanged QRS complex;
-unmodified the morphology of the P wave;
-respiratory sinus arrhythmia disappears on the inhale.
Extrasystole (Part of Active heterotopic:)
Extrasystole is an extraordinary reduction in either the heart or its departments.
Causes: coronary heart disease, myocardial dystrophy, myocarditis, hyperthyroidism, menopause, various intoxications, Smoking, the abuse of strong tea, coffee, violations of electrolyte metabolism (especially potassium deficiency), cardiomyopathy, GB, metabolic syndrome.
In any part of the conducting system of the heart can occur aberrant (ectopic) foci of excitation. The pulses from such sources can cause extra contraction of the heart. Distinguish supraventricular (atrial and nodal) and ventricular (idioventricular) beats.
Clinic: – patients experience some disruptions in the heart or a stop followed by a strong blow; – anxiety, fear; – weakness, dizziness, – blurred vision (“seeing dark spots”, “blackouts”).
Classic ECG signs of atrial arrhythmia:
1) premature appearance of the P wave (earlier than the duration of the preceding RR) in premature complex;
2) deformation and/or changing the polarity of the P wave premature beats;
3) the presence of unchanged ventricular QRST complex is premature as the P wave;
4) incomplete compensatory pause.

ECG signs of nodal extrasystole:
1) premature appearance of unchanged ventricular complex QRS”;
2) the absence of the P wave;
3) may be negative as the P wave in leads II, III and aVF after the QRS complex of extrasystole ;
4) incomplete or complete compensatory pause.
ECG signs of ventricular extrasystole:
1) premature appearance of an extraordinary altered ventricular QRS complex (it is extended ≥0,12 s, and strain);
2) the location of segment S(R)-T and T wave of beats discordance to the direction of the main wave of the QRS complex;
3) there is no P wave before ventricular contraction;
4) the presence of a complete compensatory pause.
The compensatory pause is an electrophysiological concept describing the degree of influence of the beats on automaticity (sinus node discharge) after the early contraction. The concept of – compensatory pause comprises two intervals:
1) the coupling interval (premature interval), the distance from the last sinus complex to the beats;
2) interval, called the pause post extra systolic, i.e. the distance from the beats to the next sinus complex. The sum of these two distances is a compensatory pause. Up to the duration of the compensatory pause can be complete or incomplete.
A complete compensatory pause usually accompanies all ventricular extrasystoles of classic character and part of the nodal escape (nodal extrasystoles). Under these conditions the compensatory pause is equal to two preceding RR intervals of sinus rhythm.
Incomplete compensatory pause usually occurs in classic atrial and nodal extrasystoles, its length is less than the two preceding RR intervals of sinus rhythm. There are two types of atypical ventricular extrasystoles in which there is no classical compensatory pause is inserted ventricular extrasystoles and late ventricular extrasystoles.
In modern electrophysiology in characterizing extrasystole there are a number of old terms, which is sometimes used to assess clinical significance. Monotopic are ectopic beats (extrasystoles) originating from a single source of excitation and having an identical coupling interval (its permissible variations of 0.02 – 0.04c.)
Polytopic are ectopic beats originating from different foci of excitation with different coupling interval (fluctuations of 0.06 – 0.08). The shape of the beats can be monomorphic, i.e., identical, and polymorphic, i.e. different. At the moment, to simplify specifications we use the following terms: monofactorial (equal interval of coupling and form) and polyactorial (of different shape or interval of coupling).
On the frequency there are isolated single ectopic beats, pairs (two in a row), group (3 to 4 in a row) and short unstable paroxysms (of 5 and more). Term allorhythmia has significant clinical importance this is a regular alternation of extrasystoles and sinus rhythm. If the contraction is repeated after each normal reduction is bigeminy (see figure). If for every two normal beats is trigeminy, etc.
Clear prognostic significance of supraventricular extrasystoles does not exist. All electrophysiologs agree that we must treatment supraventricular extrasystoles arising on the background of tachycardia in the acute phase of cardio – vascular diseases and with poor subjective tolerability.
For ventricular extrasystoles a special predictive classification developed. This is the advanced classification of Laun (Ryan) and Merberg`s classification. The higher the grade the worse the prognosis.
Classification of ventricular extrasystoles in the modification M. Ryan (1975)
no extrasystoles for 24 hours monitoring;
1 – no more than 30 for any hour of monitoring;
2 – more than 30 for any hour of monitoring;
3 – polymorphic extrasystoles;
4A – monomorphic pair;
4B – polymorphic pair;
5 – short runs of ventricular tachycardia (>3 consecutive).
Classification of ventricular extrasystoles by Merberg (1984)
Quantitative characteristic:
0 – no extrasystoles;
1st class rare – up to 1 hour; 2 CL infrequent – 1 to 9 per hour;
3 CL intermediate – 10-29 per hour;
CL. 4 frequent – >30 per hour.
Morphological characteristics:
CL. A – monomorphic (monofokalnye);
CL. B – polymorphic (polyfucose);
CL. C – pair, volley, return, allorhythmic;
CL. D – unstable ventricular tachycardia;
CL. E – sustained ventricular tachycardia.



PAROXYSMAL TACHYCARDIA (Active heterotopic:)
Paroxysmal tachycardia is suddenly beginning and as suddenly ending attack of increase heart rate to 140-250 per minute while maintaining, in most cases, regular rhythm. These transient attacks can be unstable (shorter than 30 s) and persistent (lasting more than 30).
Reasons (can be organic and physiological): puberty, physical and psychological stress, myocardial infarction, myocarditis, valvular heart disease, heart failure, hyperthyroidism, adolescence, pregnancy,
menopause, abuse strong coffee, alcohol, Smoking, diseases of the stomach, gall bladder, kidneys, severe intoxication and electrolyte imbalance.
Currently, there are two main mechanism of paroxysmal tachycardias:
1) the mechanism of re-entry of the excitation wave (re-entry);
2)increasing automaticity cells of the conducting system of the heart in ectopic centers of II and III order. There is ectopic active center in the heart conducting system occurs, which becomes the pacemaker for some time, as the frequency of its impulses is more than the frequency of the sinus node. Distinguished: atrial, nodal and ventricular form of paroxysmal tachycardia.
Paroxysmal supraventricular tachycardia
Electro cardiology of atrial and nodal tachycardia paroxysmal form often combine the concept of supraventricular (supraventricular) tachycardia, especially because medical treatment of these forms is largely similar. Causes more functional, less organic.
In practical Clinic: suddenly beginning and suddenly ending an attack of the heart (interruptions); – shortness of breath; – compressive pain in the heart region; – the feeling of fear; – weakness, dizziness. After relief of the attack the patient often feels a sense of pleasant ease, accompanied by a feeling of weakness. After an attack is usually a large amount of clear urine.
ECG signs of atrial paroxysmal tachycardia:
1) the same R-R intervals with the presence of atrioventricular conduction (positive or negative of the P wave before each QRS complex);
2) rhythm frequency more than 150 per minute (frequency rate can be measured as the RR interval, and RR interval);
3) stable, somewhat elongated PQ interval;
4) normal, unmodified ventricular complexes (the same as in sinus rhythm;
5) there is no change in the ST segment and T wave
ECG signs of nodal paroxysmal tachycardia:
1) the heart rate ranges from 170 to 220 beats per minute (calculated on RR intervals);
2) normal unmodified ventricular complexes QRS, similar to the sinus QRS complexes, recorded before the attack of paroxysmal tachycardia;
3) absence of the P wave or the presence of retrograde P wave before or after each QRS complex;
4) no changes of ST segment and T wave


Ventricular paroxysmal tachycardia
True ventricular tachycardia is usually more severe than supraventricular, with focal cerebral symptoms, phenomena of cardiogenic shock, acute heart failure and its reasons almost always have an organic origin. Requiring urgent intensive care intervention in response to severe hemodynamic instability.
ECG signs of ventricular paroxysmal tachycardia:
QRS. 1) wide (≥0.12 QRS), strain;
2) rhythm frequency of more than 130 beats per minute;
3) discordant (opposite direction of the main ventricular prongs) change of ST segment and T wave;
4) the absence of the P wave before or after QRS;
5) in true ventricular tachycardia, especially during prolonged ECG, can meet the so-called “ventricular capture” is premature narrow QRS complexes with sinus tooth R. This is a sign used in the differential diagnosis of tachycardias with a wide QRS complex.

ATRIAL FLUTTER
Circular circulation of excitation on the foci of ectopic atrial regular or irregular conduct to the ventricles. Pathognomonic frequency of the pulses in the centers of excitation of 220 – 350 per minute.
The direct mechanisms leading to very frequent excitation of the Atria when the flutter is either increased automaticity cells of the conducting system or the mechanism of re-entry wave excitation –
re-entry, when in fibrillation, the conditions for a long period of rhythmic circulation of the circular excitation wave. Unlike atrial fibrillation, when atrial flutter contractive function persists.
Classic ECG signs of atrial flutter (by Kushakovskij M. (1998):
1) frequent – up to 200-400 per minute – regular, similar to each other atrial F waves, with a characteristic sawtooth shape (leads II, III, aVF), simulating the lack of contour lines;
2) the presence of a normal unmodified ventricular complexes QRS (if not the original blockade legs);
3) each gastric complex is preceded by a certain number of atrial waves F (2:1, 3:1, 4:1 etc.) at regular (correct) form of atrial flutter. The irregular (incorrect) form, the number of these waves may vary.

The so-called atypical forms of atrial flutter. The frequency of the waves F is in the border zone 200 – 220 in 1 minute, while the polarity of the F waves in II, III, аVF negative in V1 and positive V2. This so-called levomitsetina form, when the ectopic focus is in the left atrium. This type of atrial worst amenable to medical and surgical treatment.
Classical type of flutter described above, is more common. While the point of excitation is located in the right atrium, in the so-called isthmic area, so its old name is isthmus flutter. This form of responds well to surgical atrial ablation.
ATRIAL FIBRILLATION
This chaotic activity of the Atria with irregular ventricular responses due to violations of atrioventricular conduction.
This is the most frequent rhythm disturbance in adults. Its prevalence increases with age: at age 60 it is 1.5%, over the age of 80 years is about 9%. Cause rhythm disturbances –
multiple foci of excitation with a high frequency of formation of pulses, operating on the mechanism of re-entry. Most often the lesions are located in the left atrium, close to the mouth of the pulmonary veins.
In 90% of cases the cause of atrial fibrillation is atherosclerosis with the development of coronary heart disease, congenital and acquired heart diseases (most often mitral valve disease), chronic heart failure, thyrotoxicosis, pulmonary embolism, COPD.
The reason can be called overdose drugs (cardiac glycosides, adrenaline, noradrenaline, etc.), medical manipulation (reflex to sensing of the heart cavities), operations on organs of thoracic and abdominal cavities, alcohol, intoxication by carbon monoxide, electric shock, lightning.
In 15% of cases, atrial fibrillation occurs for no apparent reason, this so-called idiopathic form, where is a triggering factor of atrial premature beats.
There are following forms of atrial fibrillation: – paroxysmal: duration of attack from 30 sec. to 2 days; – persistent: duration of attack of more than 7 days at this rhythm disturbance can be eliminated either with medication, or cardioversion; permanent or chronic: lasts more than a year, the disruptions cannot be eliminated with conventional methods.
Clinic: –
-shortness of breath;
-angina;
– palpitations and interruptions in heart work;
-sudden weakness;
– fainting, until he lost consciousness;
– dizziness;
– the fear of death.
ECG signs of atrial fibrillation:
1) no in all electrocardiographic leads is the P wave;
2) the availability throughout the cardiac cycle chaotic f waves, having different shape and amplitude (f waves better recorded in leads V1, V2, II, III and aVF), pathognomonic frequency of the waves f – 350 – ;׳ 700
3) irregularity of the ventricular complexes QRS (various durations R-R), QRS complexes have, in most cases, the normal invariant form.
Depending on the size of waves distinguish between large and small wave forms of atrial fibrillation. When large wave form – the shape of the wave amplitude f exceeds 0.5 mm, the frequency 350-450 per minute.
This form occurs more often in patients with marked hypertrophy of the Atria, for example, in mitral stenosis. When small wave form of atrial fibrillation frequency of the wave f reaches 600-700 per minute,
their amplitude is less than 0.5 mm, Irregular waves are more pronounced than in the first embodiment. Sometimes f waves are generally not visible on the ECG in any of the 12 electrocardiographic leads, then remove the lead V3R (right breast). This form of atrial fibrillation often occurs in older people with cardiosclerosis.
Depending on the frequency of occurrence of the QRs complexes, there are three forms of atrial fibrillation: 1) tachyarrhythmic (average frequency of reductions of ventricles above 90 per minute;
the average frequency believe in 10 consecutive R-R intervals in one lead); 2) bradiaritmicheskuyu (average frequency of contractions of the ventricles does not exceed 60 per minute); 3) normalities (average frequency of reductions of ventricles 60 to 90 per minute).
Clinically most unfavorable form is tachyarrhythmic

You should remember that patients on the background of atrial fibrillation we can`t talk about supraventricular extrasystole, there may be registered only ventricular extrasystole.
Ventricular fibrillation
Ventricular fibrillation is a terminal arrhythmia with asynchronous electrical activity of individual groups of muscles of the ventricles and the termination of the systole of the ventricles. In the ECG is manifested by irregular waves of varying amplitude and shape. It ends with asystolia.