Infectious safety Nosocomial infections Prevention of nosocomial infections
Infectious safety Nosocomial infections Prevention of nosocomial infections
Nosocomial infections: (hospital) – is any clinical microbial disease, affecting the patient as a result of hospitalization or hospital visits in order to receive treatment.
Nosocomial infection is a disease developed in a patient 48 hours after admission, and healthcare worker involved in the treatment and care of patients in the hospital.
The problem of nosocomial infection and infection control is a priority for a number of reasons, which include the following:
- mortality of nosocomial infection in medical hospitals took the first place;
- infection acquired patients in the hospital, greatly increases the cost of his treatment, because it involves the use of costly antibiotics and increases the duration of hospitalization;
- infection – the main cause of illness and death in newborns, especially premature (for example, 25% of premature infants in the intensive care unit develops sepsis, making the frequency of death 2 times higher and hospitalization longer);
- disability due to nosocomial infection has significant financial problems for the patient and his family.
- In the United States of 120000 or more patients infected with NI, killed about 25% of cases and, according to experts, NI represent the leading cause of deaths. Obtained in recent years evidence suggests that NI significantly lengthen the duration of stay of patients in hospitals, and caused damage every year is from 5 to 10 billion dollars in the United States.

What is Infection ?
- «Infection» is a biological phenomenon characterized by the interaction of a pathogenic microorganism with a macroorganism (human).
- «Infectious process» – a complex of adaptive reactions of the organism in response to the introduction and proliferation of the pathogen. (Reactions aimed at restoration of homeostasis and disturbed biological equilibrium with the environment).
- Microorganism that can cause infectious disease is called a pathogen.
Properties of pathogen:
- Invasiveness – the ability of the pathogen to penetrate through the skin and mucous membranes into the internal environment of a macroorganism.
- Toxigenicity — the ability of microbes to produce toxins.
CHAIN OF INFECTION
Main Components of the chain of infection (simple version).
1)Infectious agent (pathogen)
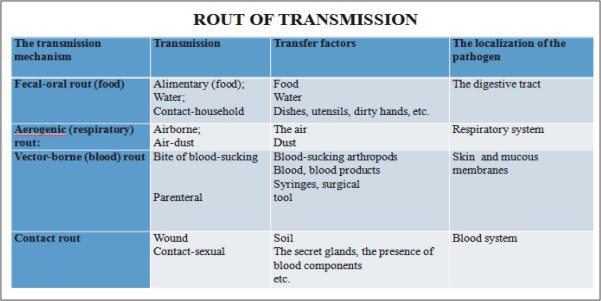
2)Rout of transmission
3)Susceptible host.
CHAIN OF INFECTION
The presence of a pathogen does not mean that an infection will begin. The process resulting in an infection is referred to as the chain of infection.
Components of the chain include:
1)Infectious agent (pathogen). Reservoir – a place where microorganisms survive, multiply, and wait to transfer to a susceptible host. Common reservoirs are humans and animals, insects, food, water. Frequent reservoirs for health care-associated infections include health care workers (especially their hands), patients’ body excretions and secretions, equipment, and the health care environment. There are two types of human reservoirs: those with acute or symptomatic disease and who show no signs of disease but are carriers of the disease. Human can transmit microorganisms in either case. Portal of exit. After microorganisms find a site in which to grow and multiply, they must find a portal of exit if they are to enter another host. Microorganisms exit through a variety of sites such as skin and mucous membranes, respiratory tract, gastrointestinal tract, urinary tract, and in blood.
2)Rout of transmission. Many times there is little that you are able to do about the infectious agent or the susceptible host, but by practicing infection prevention and control techniques, such as hand hygiene, you interrupt the rout of transmission. Portal of entry. Organisms are able to enter the body through the same routes they use for exiting. Common portals of entry include broken skin, mucous membranes, genitourinary (GU) tract, gastrointestinal (GI) tract, and respiratory tract.
3)Susceptible host. Susceptible to an infection depends on the individual’ degree of resistance to pathogens. Although everyone is constantly in contact with large numbers of microorganisms, an infection does not develop until an individual becomes susceptible to the strength and numbers of those microorganisms.
Types of Nosocomial Infection
There are TWO FORMS OF NOSOCOMIAL INFECTION (classification):
- Endogenous infection (self-infection, or auto infection).
- The causative agent of the infection is present in the patient at the time of admission to hospital but there are no signs of infection. The infection develops during the stay in hospital as a result of the patient’s altered resistance
ü hematogenic way – infection spreads with blood flow.
ü lymphogenic way – infection spreads with lymph flow.
- Exogenous infection (Cross-contamination followed by cross-infection):
- During the stay in hospital the patient comes into contact with new infective agents, becomes contaminated, and subsequently develops an infection.
Sources of Exogenous hospital infection – sick man:
1) patients with acute or chronic form of infectious diseases.
2) infection carriers (carriers do not get sick, but they can pass the infection to others);
3) medical staff.
THE PREVENTION OF NOSOCOMIAL INFECTION:
Two basic principles govern the main measures that should be taken in order to prevent the spread of nosocomial infections in health-care facilities:
1.early detection of source of infection:
- Identification of infectious patients on admission
- Isolation of infectious patients
- Preventive medical examination of medical personnel
- Cut off any route of transmission of infection (Aseptic techniques):
- Clinical hygiene of medical staff
- Collection and disposal/decontamination of waste
- Cleaning of premises
- Disinfection
- Sterilization
- ASEPSIS
Efforts to minimize the onset and spread of infection are based on the principles of Aseptic technique. Aseptic technique is an effort to keep the patient as free from exposure to infection-causing pathogens as possible. The term asepsis means the absence of disease-producing microorganisms. The two types of aseptic technique are medical asepsis and surgical asepsis.
- Medical asepsis includes procedures used to reduce the number of and prevent the spread of microorganisms. Hand hygiene, barrier techniques, and routine environmental cleaning are examples of medical asepsis.
- Surgical asepsis, or sterile technique, includes procedures to eliminate all microorganisms from an area. Sterilization destroys all microorganisms and their spores.
Nurses in the operating room, labor and delivery, and at the bedside practice sterile technique when using sterile instruments and supplies for patients care.
Surgical asepsis demands the highest level of asepsis technique and requires that all areas be kept free of infectious microorganisms.
Health care workers are responsible for providing a safe environment for patient. It is easy to forget key procedural steps or to take shortcuts that break aseptic procedures when hurried. Failure to follow proper techniques place patients at risk for an infection that can seriously impair their recovery and may even lead to death.
CLINICAL HYGIENE OF MEDICAL STAFF
- Keep your body clean.
- Wear special clothes: a medical bathrobe, a medical cap, shoes.
- Use protectors: gloves, mask, goggles, safety glasses.
- Wash your hands
Medical gown (bathrobe)
- Special clothes of a modern medical worker – a medical gown
- There are many microbes on clothes. Caps, bathrobe, trousers and shoes are most contaminated with microbes.
- On medical bathrobe the hospital microbes can be found in a few hours of wearing, especially on the sleeves, on the area of abdomen and on the hips.
- It is necessary to have a special room where a doctor can change clothes.
- Work clothing and personal clothing must be kept separately.
- Doctors must wear a bathrobe over their own clothes and it must fully cover personal clothes of a doctor.
- Sleeves must be short in order to make hand wash easier.
Medical cap
- Hair – is a huge area that can collect and then distribute microorganisms.
- It is necessary to wear a cap in the surgical department. The hair must be hide under the medical cap.
- It is necessary to replace medical cap daily.
Shoes (footwear)
- Footwear must be closed in order to protect feet against contact with blood and other biological fluids. Shoes must be made of nonwoven fabric, so that it can be exposed to cleaning and disinfection.
Protectors
- Working in aseptic and infected areas medical staff should wear protective disposable masks. Mask should be replaced every 2 hours, and after each surgery.
- All the dirty work must be done in oilcloth aprons. Apron is worn over the bathrobe.
- In case of contact with the patient doctors must wear rubber disposable gloves.
HAND WASHING
- Hands – are the most likely source of infection. It is necessary for every medical worker to care for them.
- Skin microflora
Resident microflora (constant). It is impossible to destroy completely this microflora.
Transient microflora (temporary). It is received through any contact with the environment.
- As the hands of health-care workers are the most frequent vehicle of nosocomial infections, hand hygiene—including both hand washing and hand disinfection—is the primary preventive measure. Thorough hand washing with adequate quantities of water and soap removes more than 90% of the transient, i.e. superficial, flora including all or most contaminants. An antimicrobial soap will further reduce the transient flora, but only if used for several minutes.
The points to be kept in mind while washing hands are:
- Cut short nails. A long nail will give roof to the dirt and microorganisms.
- Remove the jewelry of any type. Open the tap and wet hands and forearm. Always hold the hands below the elbow level, because hands are considered to be more contaminated then the elbows, hence the water should flow from the area of least contamination (the elbows) to the area of more contamination (the hands).
- Apply soap or detergent.
- Wash hands thoroughly. Make sure that the interdigital space are cleaned by washing each finger separately. Use brush to dislodge the dirt from under the nail beds.
- Rinse hands by keeping the hands well below the elbow level. The water flows from elbow to the hands.
- Repeat the procedure (application of soap and rinsing with water) to ensure thorough cleanliness.
- Dry the arms and hands, starting at the elbows and working towards the hands.
- Discard the towel.
- Turn off the water tap using a paper towel because the handle is contaminated.
- While washing, if the hands touch the sink or other objects accidentally, the whole procedure needs to be repeated.
Algorithm hygienic washing of hands:
- Moisten hands with water. To take of a little liquid soap, to lather his hands.
- Рosition of the hands – palm to palm. Rub together 10 seconds.
- Рosition – right palm over back of the left hand with intertwined fingers. Rub 10 seconds.
- Рosition – left palm over back of the right hand with intertwined fingers. Rub 10 seconds.
- Рosition of the hands – palm to palm. Rub the interior surface of the fingers. Rub 10 seconds.
- Рosition – the back of the fingers to the palm of the other hand. Rub 10 seconds.
- Rub the thumb with the palm of the other hand by rotational movement.
- Рosition. Circular motion with the tips of the fingers on the palm.
- Repeat each movement not less 5 times.
Technique putting on sterile gloves
Equipment: pack of sterile gloves.
Algorithm:
- Pull out and unfold the package with gloves.
- Take the glove for a top with left hand so that the fingers touched the inner surface of the glove.
- Fingers of the right hand connect and to enter them into a glove.
- Enter the fingers into glove, not breaking her lapel (cuff).
- Enter the 2nd, 3rd and 4th fingers of the right hand under a lapel (cuff) of left glove from the outer side. The first finger of the right hand should be pointing towards the 1-st finger of the left glove.
- Keep the left glove by 2-nd, 3-rd and 4-th fingers the of the right hand vertically. Fingers of the left hand connect and to enter them into a glove.
- Straighten the lapel of left glove, having pulled it on a sleeve.
Enter the 2nd, 3rd fingers of the left hand under a lapel (cuff) of right glove from the outer side, straighten the lapel of right glove, having pulled it on a sleeve.
!! If one glove was damaged, it is necessary change both, because you can’t take off one glove, not contaminating another.
Removal of Gloves
Equipment: pack of sterile gloves.
Algorithm:
- To make a lapel by fingers of the right hand on left glove, touching only of the outer side.
- To make a lapel by fingers of the left hand on right glove, only of the outer side.
- To take off a glove from the left hand, turning inside out, pulling by the lapel.
- Hold the removed glove right hand.
- Take the right glove for the lapel on the inside.
- To take off a glove from the right hand, turning it inside out, pulling by the lapel.
- To place gloves in the container with a disinfectant.
MEDICAL WASTE, classification
- CLASS “A”. Not dangerous waste.
- CLASS «B”. Dangerous waste.
- CLASS «C». Extraordinarily dangerous waste.
- CLASS «D”. Toxicologically dangerous waste.
- CLASS «E». Radioactive waste
MEDICAL WASTE
CLASS “A”. Not dangerous waste
It is non-toxic waste, not having contact with body fluids of patients, infectious patients.
Not dangerous CLASS “A” is formed:
- In the wards in all structural units of hospital.
- In administrative quarters
- In the buffet, in the nutrition unit.
- In the territory of hospital
!!! Territory infectious, dermatovenerologic, tuberculous hospitals is exception.
Not dangerous CLASS «A» is collected in a disposable package (packages, cans) white colour.
CLASS «B”. Dangerous waste. Dangerous waste is potentially infected waste, contaminated by secretions and blood of patients.
Places of formation:
- Waste from any inpatient Department contaminated biological fluids
- Treatment rooms,
- Dressings rooms,
- Manipulation rooms
- Operating rooms
- Pathoanatomical department
- Diagnostic Department (laboratory)
- Food waste from infectious disease department
Dangerous waste CLASS «B» is collected in a disposable hermetic package (packages, cans) yellow colour.
Marking – Dangerous waste. Class «B», code of department, name of the hospital, date, name of the responsible for collection of waste.
CLASS «C». Extraordinarily dangerous waste
CLASS «C» is waste contacted with sick of especially dangerous infections.
Places of formation waste CLASS «В»:
Departments for patients with especially dangerous and quarantine infections:
- Tuberculosis hospital and departments
- Infectious and dermatovenerologic departments
- Mycological hospitals
- Materials from patients with anaerobic infection.
Waste CLASS «В» is collected in a disposable hermetic package red colour (packages and hard packing).
Marking – “Extraordinarily dangerous waste. Class C,code of department, name of the hospital, date, name of the responsible for collection of waste.
CLASS “D” – Toxicologically dangerous waste
Waste CLASS «D» is
- Expired medicines
- Toxic drugs (cytostatic drug and other chemicals, mercury-containing objects,
- Used disinfectants,
- Medical apparatus and equipment.
Waste CLASS «D» is collected in a disposable hermetic package (packages, cans) black colour.
Marking – Waste. Klass D, code of department, name of the hospital, date, name of the responsible for collection of waste.
CLASS «E». Radioactive waste
Waste CLASS «E» is all kinds of waste containing radioactive components.
Places of formation:
- Diagnostic laboratories or departments
- Radioisotope laboratory
- X-ray rooms
Collection, storage and removal waste of this class carry out in accordance with the rules for work with radioactive substances.
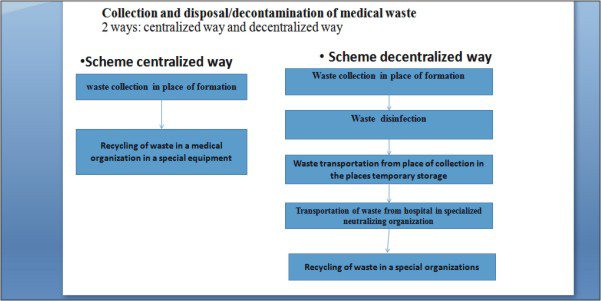
Collection and disposal decontamination of medical waste 2 ways centralized way and decentralized way
Disinfection
- Disinfection – is the destruction of pathogenic and conditionally pathogenic microorganisms in the air, on-site equipment and medical products in the treatment-and-prophylactic institution.
Objectives of disinfection:
- Prevention of nosocomial infections.
- Interruption ways of transmission infection, the destruction of the infectious agent.
OBJECT of DISINFECTION
1.All types of surfaces in hospital (walls, floor, furniture, etc.).
2.Medical products.
3.Hands of medical personnel.
4.Skin of the patient.
5.Objects for nursing.
6.Indoor air.
7.Bed linen.
8.Tableware.
9.Medical waste and other objects that may be factors of transmission of nosocomial infections.
TYPES OF DISINFECTION:
1.PREVENTIVE DISINFECTION is aimed at preventing the occurrence of infections, in the absence of the focus of infection. It is provided in the treatment-prophylactic institution, is carried out by medical personnel (orderlies, junior medical personnel, nurses).
- Preventive planned disinfection is carried out in the hospital continuously; is carried out according to the plan maked accordingly with peculiarity of hospital departments.
- Preventive disinfection on epidemic indications is carried out with the occurrence of nosocomial infection in one from hospital departments (or in one from chambers). For example, the patient is ill by the influenza in the one ward. Purpose – prevent the spread of infectious agents in other departments.
- Preventive disinfection on sanitary and hydenic indications is carried out once at the contamination.
- FOCAL DISINFECTION:
- Focal current disinfection – is conducted constantly in a treatment-prophylactic institution or at home surrounded by the patient after detection in a patient of nosocomial infection and before discharge (or transfer to another Department/hospital).
- Focal final disinfection – is carried out once after discharge or death, the hospitalization the patient in an infectious hospital.
Methods of disinfection:
1.Mechanical method (soil removal):
- wet cleaning rooms and equipment
- tapping out of clothes, bedclothes
- dust removal, repair of rooms
- scrubbing the hands of personnel.
- Chemical method – with using disinfectants.
- irrigation
- wiping
- total immersion
- spraying
- Physical method – thermal, most reliable and harmless to personnel.
- using of sunlight
- bactericidal lamp
- ironing, calcination by high temperature
- incineration of waste
- boiling
- pasteurization
- tyndalization (fractional pasteurization)
- air method (in a dry-heat tool cabinet)
- steam method (steam treatment – autoclaving)
- processing the objects in special chamber by high pressure.
- Combined method – a different combination of physical and chemical methods of disinfection.
- Biological method – the destruction of pathogens using microbies-antagonists (bacteriophages).
Disinfection efficiency depends on:
- the stability of the microorganism
- quantity of microbies
- concentration of disinfectant
- presence of organic substances on the objects (blood, feces, sputum)
- exposition
- method of processing (wiping, irrigation, total immersion in disinfectant)
- texture of processed objects
Quality control of disinfection
- Visual control – the assessment of sanitary condition of the rooms, result current and general cleaning.
- Chemical control – determination of the concentration of ready disinfectants, express test – paper test-strips and control color scale.
- Bacteriological control – taking wash-out and inoculation. This analysis is conducted by laboratorian from Hygiene and Epidemiology Center.
Types of disinfectants:
1.For disinfection of medical products.
- For disinfection of rooms, furniture and objects of nursing for patients.
- Dermal antiseptics.
Requirements for disinfectants:
- Wide spectrum of actions
- low toxicity
- Good solubility in water
- Activity in small concentrations
- Minimum time of effective exposure
- Stability at the storage (expiration date)
- Convenient transportation
- Disinfectant should not damage
processed objects.
Also Read this Article
Mensuration Cycle Female Reproductive System
Safety rules when working with disinfectants
- Proper storage of disinfectants.
- Labelling – the name, appointment, date of manufacture and expiration date.
- Observance the rules of personal hygiene (a special gown, kerchief, respirater, goggles, rubber gloves, removable shoes)
- Use ventilation at the preparing solutions
First aid for poisoning by disinfectants
- After contact with skin – wash them immediately with water.
- Eye contact – rinse immediately with water, to inject drops into the eye (30% albucid, 2% novocaine solution – 1-2 drops.
- In case of irritation of the respiratory tract – to go to another room or fresh air, rinse the mouth and nasopharynx with water (if necessary appoint hearty, soothing, antitussives remedies).
STERILIZATION
Sterilization – is the complete destruction of microorganisms and their spores by exposure to physical factors and chemicals matters.
All products are subjected to sterilization in contact with a wound surface, blood, certain types of medical instruments.
The main stages of MEDICAL TOOLS processing :
1 Stage. disinfection
2 Stage. pre-sterilization processing
3 Stage. control of sterilization processing
4 Stage. sterilization
1 STAGE. DISINFECTION OF INSTRUMENTS OF MEDICAL APPOINTMENT
Equipment:
- disinfectant solution
- 1 сontainer (for lavage)
- 2 сontainer (for disinfection)
- medical trays
- instruments after use in assembled form
1 STAGE. DISINFECTION OF INSTRUMENTS OF MEDICAL APPOINTMENT
Equipment:
- disinfectant solution
- 1 сontainer (for lavage)
- 2 сontainer (for disinfection)
- medical trays
- instruments after use in assembled form
1 STAGE. DISINFECTION OF INSTRUMENTS OF MEDICAL APPOINTMENT
Equipment:
- disinfectant solution
- 1 сontainer (for lavage)
- 2 сontainer (for disinfection)
- medical trays
- instruments after use in assembled form
Some solutions allow to wash off and disinfect the tools in 1 сontainer (2 properties at the same time).
Indispensable condition – сonduct disinfection immediately after manipulation.
- Performance the procedure. Algorithm
1.Dress the special clothing (gown, mask, gloves).
2.Prepare a disinfectant solution, pour it in the containers.
3.In first сontainer (for lavage) washed the instrument without disassembling.
4.Disassemble all instruments, immerse in 2 сontainer (for disinfection) with disinfectant solution, filling internal channels of instruments.
5.Close the container by lid. Leave at the time required for disinfection.
6.Take off the gloves, immerse in a container with disinfectant.
7.Put on other gloves, derive the instrument at the end of the exposition time.
8.Put on instrument in the medical tray.Wash out the instrument under running water.
- To prepare reusable instruments for further processing (for sterilization).
- Disposable syringes put into packet yellow colour for utilization.
- Pour out used disinfectant in sewerage.
- Take off the gloves and put in disinfectant solution, wash and dry your hands.
-
2 STAGE. PRE-STERILIZATION PROCESSIING
If the instrumentation has been in contact with mucous membranes and wounds, including operating, the disinfection insufficiently. Sterilization is required. Pre-sterilization processing is carried out before sterilization.
The purpose of pre-sterilization processing – remove all small particles, medicinal products and protein contamination remaining after the operation or manipulation.
Specially prepared solutions uses during pre-sterilization processing.
The solution includes:
- water,
- hydrogen peroxide,
- cleaning agent.
Medical instrumentation are soaked in disassembled, all items are completely submerged in the solution with the filling of all cavities.
Pre-sterilization processing. Algorithm
Equipment:
- special solution
- medical trays
- brush for washing tools
- сontainer with distilled water
- dry-heat Cabinet
- instruments after use in assembled form
Algorithm:
- Dress the special clothing (gown, mask, gloves).
- Prepare a disinfectant solution
- Immerse the instruments in special solution.
- Process the instruments by brush.
- Wash out the instrument under running water.
- Rinse tools in distilled water.
- To dry in a dry-heat cabinet.
- To reduce the time of processing surgical instruments can be used are special solutions. They allow perform the disinfection and pre-sterilization processing at the same time.
- The method of physical processing can be used to lighten the work of nurses, reduce the risk of infection contamination, reduce the processing time of surgical instruments.
- For example, apparatus of ultrasound processing.
3 STAGE. СONTROL OF STERILIZATION PROCESSING.
Quality control disinfection and pre-sterilization processing is carried out daily, under the guidance of senior nurse (biological and chemical analysis).
- 1 test. Phenolphthalein test – for the presence of detergent (pink coloration).
- 2 test. Amidopyrine test – for the occult blood (blue-green color).
If tests on blood or on the remnants of detergents is positive, the medical instruments cleans again (to negative results).
4 Stage. Sterilization
- Sterilization – is the destruction of microorganisms and their spores by exposure to physical factors and chemicals matters.
- Medical device and instruments, penetrating into sterile tissue or the vessels, contacting with blood or injectable solutions is “critical” items. They must to undergo sterilization in order to all kinds of microorganisms were destroyed.
Methods of sterilization:
1.Physical method:
- Steam,
- Air,
- Glasperlenovy,
- Ultrasonic,
- Ultraviolet radiation,
- Infra-red.
- Chemical method:
- Chemical solution,
- Gas.
Sterilization of medicine products is carried out in a centralized sterilization departments.
In clinical practice most commonly used physical method of sterilization.
- Physical steam method sterilization (аutoclaving) – processing with hot steam under overpressure.
All products are sterilized by steam under pressure, is put in special packaging:
Sterilization packaging:
1.Reusable metal sterilizing box
2.Package of two layers cotton cloth
3.Kraft paper-bags of dense paper.
All kinds of special packages are marking.
Aautoclaving
Two regimes of sterilization (for autoclaving) are recommended use in treatment-and-prophylactic institution:
1.First regime sterilization is designed for products of fabric, glass, corrosion-resistant metal. Temperature 132 ° C, pressure of 2 atm, time 20 minutes.
2.Second regime sterilization (sparing regime) is recommended for the products of thin rubber, latex and certain types of polymers. Temperature of 120° C, pressure of 1.1 atmospheric, time 45 minutes.
Hot air sterilization (in a dry-heat cabinet)
Dry-heat method – the influence of dry air; use hot-air-sterilizer with different modifications.
This type of sterilization is recommended for metal products and glass. Temperature – 180 ° C, exposition – 60 min.
Control of sterilization is carried out by indicators of temperature and pressure control.
Conduct a journal of sterilization.
Chemical method – sterilization of chemical solutions.
- This is a helper method because of a medical product cannot be sterilized in the package, after sterilization, the instruments must be rinsed by sterile fluid.
- This method is used for sterilization of thermolabile products from the material.
- For example, eye pipettes, rubber balloon for enemas.
Terms of sterility.
1.Metal sterilizing box without filter – keep 3 days.
2.Metal sterilizing box with filter – 20 days.
3.Package of two layers cotton or kraft paper-bags – to 3 days, in sterile conditions.
THEORETICAL QUESTION
- Definition of nosocomial infection. The priority problems of nosocomial infections in modern health care.
- Forms of nosocomial infection (endogenous and exogenous). Sources of nosocomial infection.
- Main Components of the chain of infection.
- The route of transmission of nosocomial infection.
- The prevention of nosocomial infection.
- Prevention of Direct Contact with the infected person (Barrier nursing)
- Clinical hygiene of medical staff.
- The rules of hand treatment (wash).
- Types of medical waste. Places of formation.
- Collection and disposal/decontamination of medical waste. 2 ways: centralized way and decentralized way. The steps of collecting waste (decentralized way).
- The definition of disinfection. Types of disinfection. Methods of disinfection.
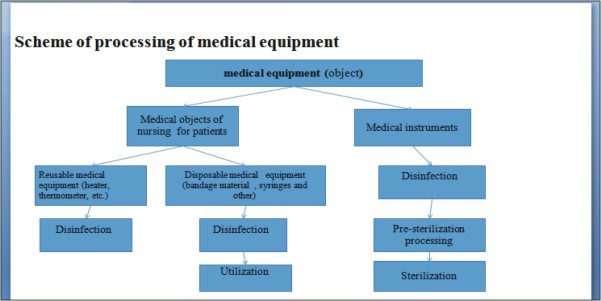
- The definition of sterilization. Types of sterilization. Scheme of processing of medical equipment.
- The main stages of medical tools processing.
PRACTICAL SKILLS
- Treating the hands by hygienic way
- Wear sterile gloves
- Remove sterile gloves
Download ppt Infectious safety Nosocomial infections Prevention of nosocomial infections



Pingback: Nursing , The organization of medical care. » Digital Hybrid Education